どこも悪くないのに胃が痛かったりむかむかする機能性胃不調(functional dyspepsia)患者206人が参加した無作為化試験でカレー香辛料ターメリック成分クルクミンがプロトンポンプ阻害剤(PPI)オメプラゾールに比肩する効果を示しました。
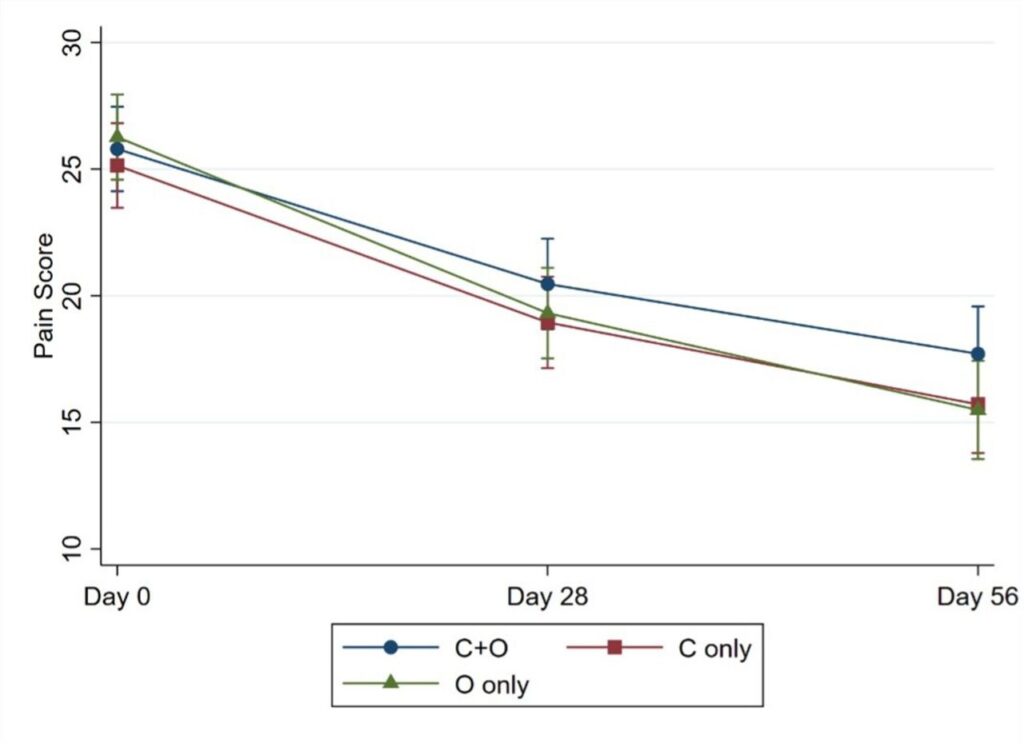
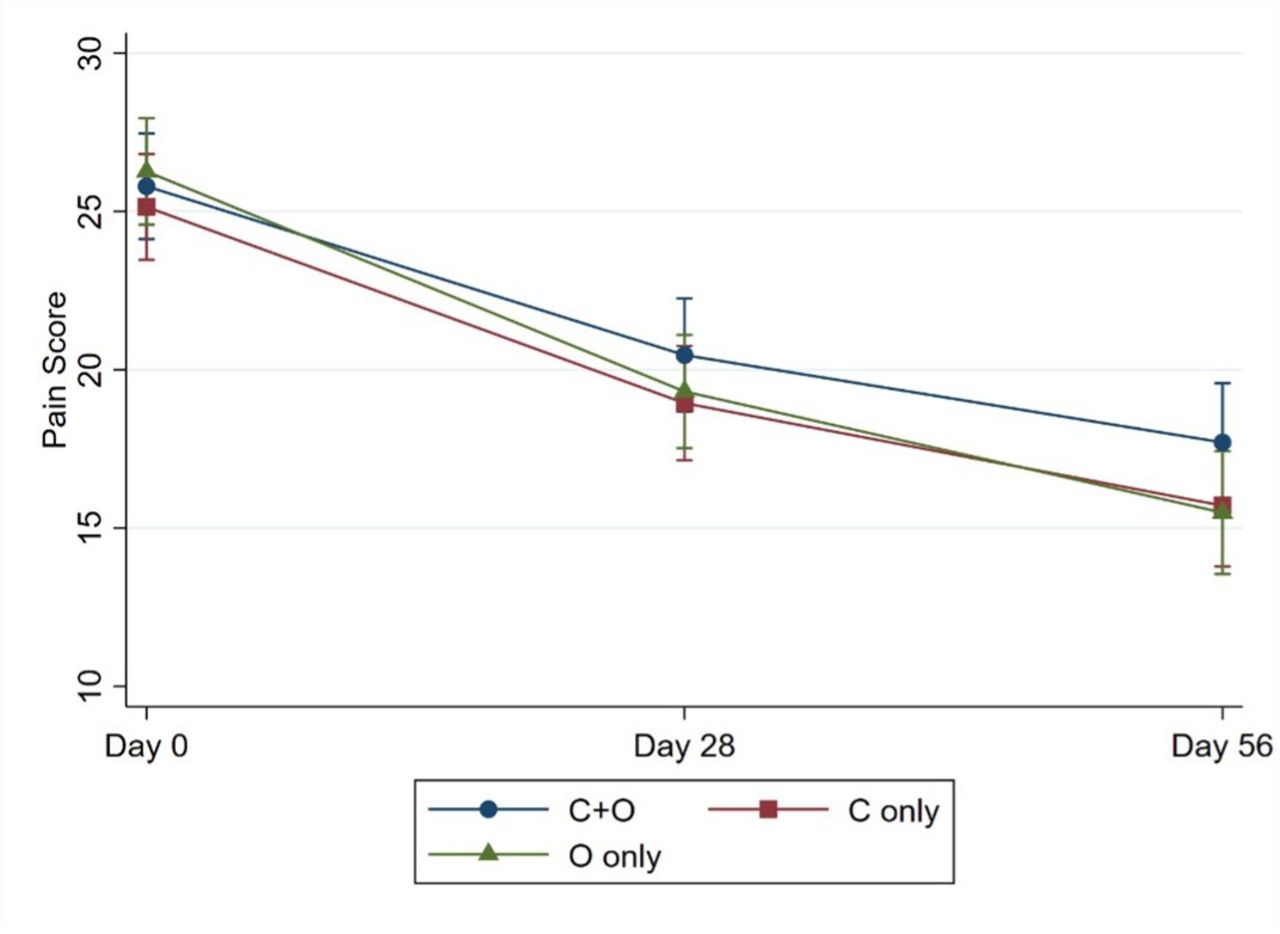
機能性胃不調の症状の検査Severity of Dyspepsia Assessment (SODA) の痛み重症度の点数がクルクミン投与群では28日時点までに5.46点下がり、オメプラゾール投与群の6.22点低下と有意差はありませんでした。痛み以外の症状の点数低下も同様に大差ありませんでした。
クルクミンとオメプラゾールの併用の一層の効果は認められませんでした。
stomach acid www.eurekalert.org/news-releases/1000882
as omeprazole—a drug used to curb excess stomach acid—for treating
indigestion symptoms, suggests the first study of its kind, published
online in the journal BMJ Evidence-Based Medicine.
Turmeric is derived from the root of the Curcuma longa plant. It contains a
naturally active compound called curcumin thought to have anti-inflammatory
and antimicrobial properties, and has long been used as a medicinal remedy,
including for the treatment of indigestion, in South East Asia.
But it’s not clear how well it compares with conventional drugs for this
indication, largely because there have been no head to head studies.
The researchers therefore randomly assigned 206 patients aged 18-70 with
recurrent upset stomach (functional dyspepsia) of unknown cause, recruited
from hospitals in Thailand between 2019 and 2021, to one of three treatment
groups for a period of 28 days.
These were: turmeric (two large 250 mg capsules of curcumin 4 times a day)
and one small dummy capsule (69 patients); omeprazole (one small 20 mg
capsule daily and two large dummy capsules 4 times a day (68 patients); and
turmeric plus omeprazole (69 patients).
Omeprazole is a proton pump inhibitor, or PPI for short. PPIs are used to
treat functional dyspepsia, the symptoms of which include feeling
excessively full after food (postprandial fullness), feeling full up after
only a little food (early satiety), and pain and/or burning sensation in
the stomach and/or food pipe (epigastric pain).
But long term use of PPIs has been linked to increased fracture risk,
micronutrient deficiencies, and a heightened risk of infections, note the
researchers.
Of the 206 patients enrolled, 151 completed the study, with 20 in the
curcumin group;19 in the omeprazole group; and 16 in the combined treatment
group, dropping out.
Patients in all three groups had similar clinical characteristics and
indigestion scores, as assessed by the Severity of Dyspepsia Assessment
score or SODA, at the start of the trial. Patients were reassessed after 28
days and then again after 56 days.
SODA scores indicated significant reductions in symptom severity by day 28
for pain (−4.83, –5.46 and −6.22) and other symptoms (−2.22, –2.32, and
−2.31) for those in the combined, curcumin alone, and omeprazole alone
groups, respectively.
These improvements were even stronger after 56 days for pain (−7.19, –8.07
and −8.85, respectively) and other symptoms (−4.09, –4.12 and −3.71,
respectively).
SODA also captures satisfaction scores: these scarcely changed over time
among the curcumin users, which might possibly be related to its taste
and/or smell, suggest the researchers.
No serious side effects were reported, although liver function tests
indicated some level of deterioration among curcumin users carrying excess
weight, note the researchers.
They acknowledge the small size of the study, as well as several other
limitations, including the short intervention period and lack of long-term
monitoring data. Further larger, long term studies are needed, they say.
Nevertheless, they conclude: “This multicentre randomised controlled trial
provides highly reliable evidence for the treatment of functional
dyspepsia,” adding that “the new findings from our study may justify
considering curcumin in clinical practice.”
Curcumin and proton pump inhibitors for functional dyspepsia: a randomised, double blind controlled trial. BMJ Evidence-Based Medicine. September 11, 2023 http://dx.doi.org/10.1136/bmjebm-2022-112231


コメント